The Duke Cancer Institute 8th Annual Scientific Retreat, held on December 3, 2021, attracted a broad array of faculty, trainees (students, residents, fellows, postdocs, etc.) and staff.
For a second year, the retreat was entirely virtual and there were no poster presentations owing to the ongoing Covid-19 pandemic.
“Hopefully, this will be the last time that we have to do it this way,” said executive director of DCI, Michael Kastan, MD, PhD, welcoming participants over Zoom.
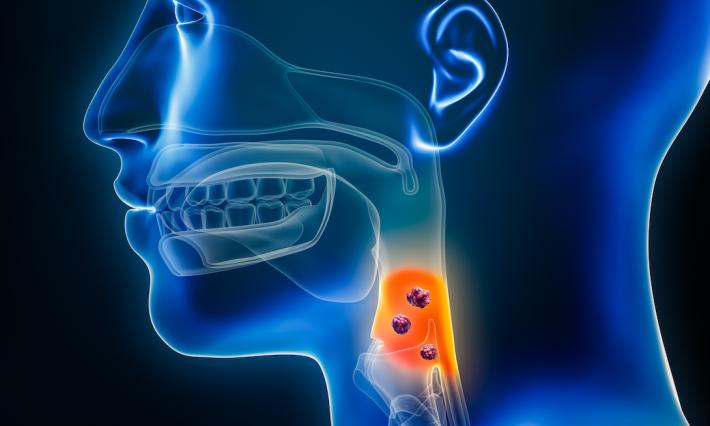
That it was virtual didn't stop a series of lively discussions from moving full-steam ahead on a full Friday afternoon on topics such as DCI cancer health equity and engagement strategies, viral lymphomas, bone loss as a CLL co-morbidity, ways around immune system evasion, cardio-protective cancer therapy, new approaches for treating head and neck squamous cell carcinoma, clues as to how cystic lesions progress to pancreatic cancer, unlocking immune dysfunction in glioblastoma, cholesterol-control drugs and cancer, and the PARP revolution.
“We have a very full agenda today with great science from Duke trainees and faculty and are also celebrating several different anniversaries. First, it's my 10th anniversary as director of the Duke Cancer Institute and I have to say it's been a real privilege of my life to be in this role and to be able to work with such extraordinary people here. And I couldn't be more proud of everything that all the staff and all the faculty have done during the time that I've been here," said Kastan. "We're also celebrating the 50th anniversary of the National Cancer Act, which was signed in 1971, and put us down the path to NCI-designated cancer centers. The Duke Comprehensive Cancer Center (now DCI) was one of the original eight."
Kastan also noted that DCI's own 50th was on the horizon.
"This year we begin celebrating our 50th anniversary. We've made a tremendous impact on cancer research and patient care in the U.S. and around the world.”